Last updated: 5/30/2015
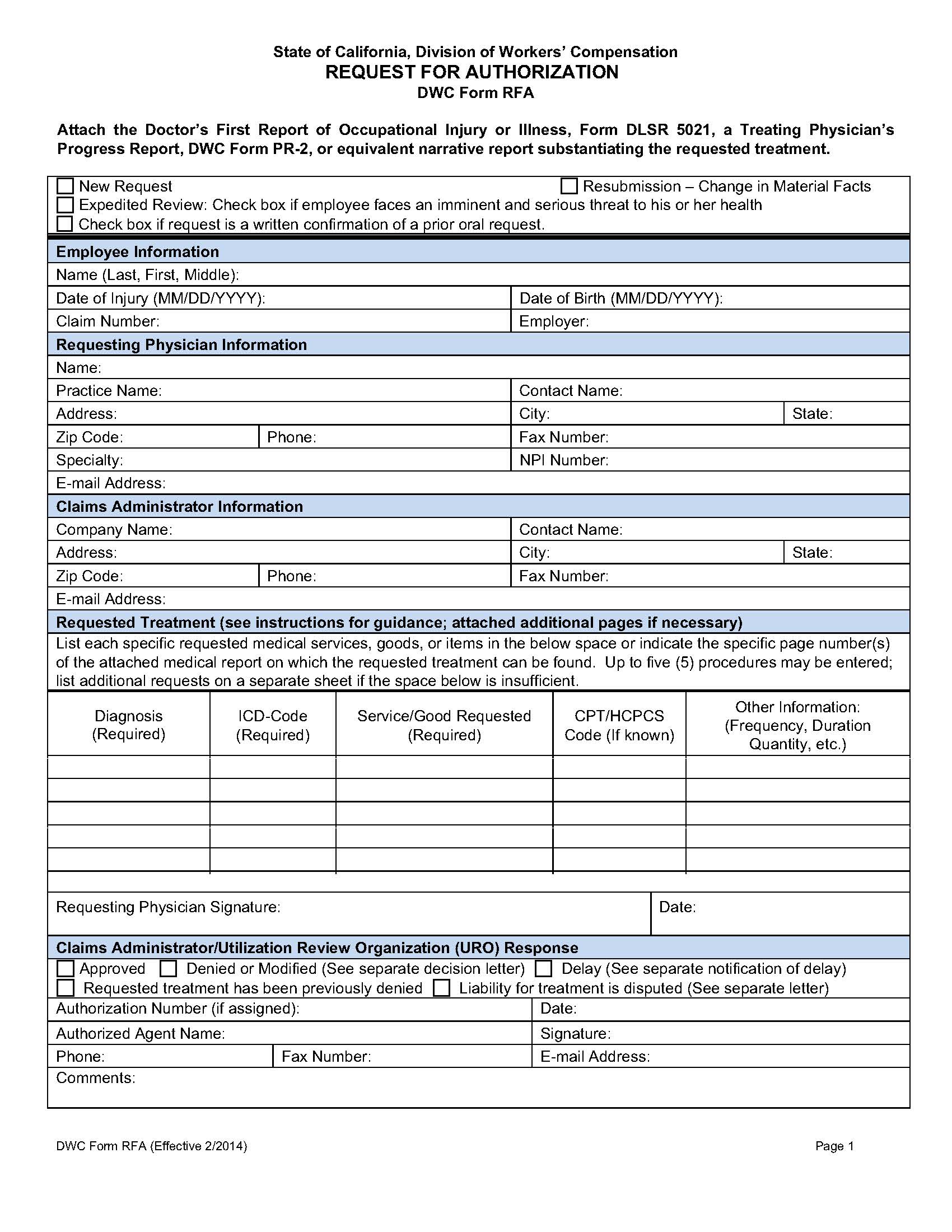
Request For Authorization For Medical Treatment {DWC RFA}
Start Your Free Trial $ 13.99What you get:
- Instant access to fillable Microsoft Word or PDF forms.
- Minimize the risk of using outdated forms and eliminate rejected fillings.
- Largest forms database in the USA with more than 80,000 federal, state and agency forms.
- Download, edit, auto-fill multiple forms at once in MS Word using our Forms Workflow Ribbon
- Trusted by 1,000s of Attorneys and Legal Professionals
Description
DWC Form RFA - REQUEST FOR AUTHORIZATION. This form is required for the employee’s treating physician to initiate the utilization review process required by Labor Code section 4610. A Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form PR-2, or equivalent narrative report substantiating the requested treatment must be attached. The DWC Form RFA is not a separately reimbursable report under the Official Medical Fee Schedule, found at California Code of Regulations, title 8, section 9789.10 et seq. www.FormsWorkflow.com
Related forms
-
 Complaint About A Workers Compensation Administrative Law Judge
Complaint About A Workers Compensation Administrative Law Judge
California/Workers Comp/General/ -
 Cover Page For Medical Provider Network Application
Cover Page For Medical Provider Network Application
California/Workers Comp/General/ -
 Declaration Pursuant To Labor Code Section 4906h
Declaration Pursuant To Labor Code Section 4906h
California/Workers Comp/General/ -
 Employers Report Of Occupational Injury Or Illness
Employers Report Of Occupational Injury Or Illness
California/Workers Comp/General/ -
 Attorney Fee Disclosure Statement
Attorney Fee Disclosure Statement
California/Workers Comp/General/ -
 Independent Medical Review Application (8 CCR 9768.10 Mandatory Form)
Independent Medical Review Application (8 CCR 9768.10 Mandatory Form)
California/Workers Comp/General/ -
 Legislative Bill Room Order Form (Official Medical Fee Schedule (OMFS))
Legislative Bill Room Order Form (Official Medical Fee Schedule (OMFS))
California/Workers Comp/General/ -
 Notice Of Dismissal Of Attorney
Notice Of Dismissal Of Attorney
California/Workers Comp/General/ -
 Notice Of Employee Death
Notice Of Employee Death
California/Workers Comp/General/ -
 Notice Of Personal Chiropractor Or Personal Acupuncturist
Notice Of Personal Chiropractor Or Personal Acupuncturist
California/Workers Comp/General/ -
 Notice Of Predesignation Of Personal Physician
Notice Of Predesignation Of Personal Physician
California/Workers Comp/General/ -
 Petition For Appointment Of Guardian Ad Litem And Trustee
Petition For Appointment Of Guardian Ad Litem And Trustee
California/Workers Comp/General/ -
 Petition For Change Of Primary Treating Physician
Petition For Change Of Primary Treating Physician
California/Workers Comp/General/ -
 Petition For Commutation Of Future Payments
Petition For Commutation Of Future Payments
California/Workers Comp/General/ -
 Petition For Permission To Negotiate A Section 3201.7 Labor-Management Agreement
Petition For Permission To Negotiate A Section 3201.7 Labor-Management Agreement
California/Workers Comp/General/ -
 Petition For Reconsideration
Petition For Reconsideration
California/Workers Comp/General/ -
 Petition To Reopen
Petition To Reopen
California/Workers Comp/General/ -
 Physician Contract Application (Independent Medical Reviewer)
Physician Contract Application (Independent Medical Reviewer)
California/Workers Comp/General/ -
 Primary Treating Physicians Permanent And Stationary Report (2005 Permanent Disability Rating Schedule)
Primary Treating Physicians Permanent And Stationary Report (2005 Permanent Disability Rating Schedule)
California/Workers Comp/General/ -
 Primary Treating Physicians Permanent And Stationary Report
Primary Treating Physicians Permanent And Stationary Report
California/Workers Comp/General/ -
 Primary Treating Physicians Progress Report
Primary Treating Physicians Progress Report
California/Workers Comp/General/ -
 Proof Of Service By Mail
Proof Of Service By Mail
California/Workers Comp/General/ -
 Public Works Payroll Reporting Form
Public Works Payroll Reporting Form
California/Workers Comp/General/ -
 Report Of Suspected Medicare Provider Fraud
Report Of Suspected Medicare Provider Fraud
California/Workers Comp/General/ -
 Request For Accommodations By Persons With Disabilities
Request For Accommodations By Persons With Disabilities
California/Workers Comp/General/ -
 Request For DWC Authorization Number
Request For DWC Authorization Number
California/Workers Comp/General/ -
 Stipulation And Order To Pay Lien Claimant
Stipulation And Order To Pay Lien Claimant
California/Workers Comp/General/ -
 Subpoena Duces Tecum (For Talent Cases Only)
Subpoena Duces Tecum (For Talent Cases Only)
California/Workers Comp/General/ -
 Subpoena Duces Tecum
Subpoena Duces Tecum
California/Workers Comp/General/ -
 Subpoena
Subpoena
California/Workers Comp/General/ -
 Arbitration Submittal Form
Arbitration Submittal Form
California/Workers Comp/General/ -
 Employers Signed Statement Of Abatement Of Regulatory And-Or General Violations
Employers Signed Statement Of Abatement Of Regulatory And-Or General Violations
California/Workers Comp/General/ -
 Employers Signed Statement Of Abatement Of Serious Violations
Employers Signed Statement Of Abatement Of Serious Violations
California/Workers Comp/General/ -
 Notice Of Verification Of Abatement Of Serious Violations
Notice Of Verification Of Abatement Of Serious Violations
California/Workers Comp/General/ -
 Application For Accreditation Or Re-Accreditation As Education Provider
Application For Accreditation Or Re-Accreditation As Education Provider
California/Workers Comp/General/ -
 Application For Appointment As Qualified Medical Evaluator
Application For Appointment As Qualified Medical Evaluator
California/Workers Comp/General/ -
 Notice Of Unavailability
Notice Of Unavailability
California/Workers Comp/General/ -
 QME Appointment Notification Form
QME Appointment Notification Form
California/Workers Comp/General/ -
 QME-AME Time Frame Extension Request
QME-AME Time Frame Extension Request
California/Workers Comp/General/ -
 Qualified Or Agreed Medical Evaluator Findings Summary Form
Qualified Or Agreed Medical Evaluator Findings Summary Form
California/Workers Comp/General/ -
 Reappointment Application As Qualified Medical Evaluator
Reappointment Application As Qualified Medical Evaluator
California/Workers Comp/General/ -
 Request For QME Panel
Request For QME Panel
California/Workers Comp/General/ -
 Request For QME Panel Under Labor Code 4062.1 Unrepresented
Request For QME Panel Under Labor Code 4062.1 Unrepresented
California/Workers Comp/General/ -
 QME Disclosure Of Specified Financial Interests
QME Disclosure Of Specified Financial Interests
California/Workers Comp/General/ -
 AME Or QME Declaration OF Service Of Medical-Legal Report
AME Or QME Declaration OF Service Of Medical-Legal Report
California/Workers Comp/General/ -
 Faculty Disclosure Of Commercial Interest
Faculty Disclosure Of Commercial Interest
California/Workers Comp/General/ -
 Declaration Regarding Protection Of Mental Health Record
Declaration Regarding Protection Of Mental Health Record
California/Workers Comp/General/ -
 QME Or AME Conflict Of Interest Disclosure Form
QME Or AME Conflict Of Interest Disclosure Form
California/Workers Comp/General/ -
 Voluntary Directive For Alternative Service Of Medical Evaluation Report On Disputed Injury
Voluntary Directive For Alternative Service Of Medical Evaluation Report On Disputed Injury
California/Workers Comp/General/ -
 Special Notice Of Lawsuit
Special Notice Of Lawsuit
California/Workers Comp/General/ -
 Substitution Of Attorneys
Substitution Of Attorneys
California/Workers Comp/General/ -
 Application For Adjudication Of Claim (Death Cases)
Application For Adjudication Of Claim (Death Cases)
California/Workers Comp/General/ -
 Addendum To Application For Adjudication Of Claim To Identify Legal Entity
Addendum To Application For Adjudication Of Claim To Identify Legal Entity
California/Workers Comp/General/ -
 Pre-Trial Lien Conference Statement
Pre-Trial Lien Conference Statement
California/Workers Comp/General/ -
 Walk Through Appearance Sheet
Walk Through Appearance Sheet
California/Workers Comp/General/ -
 Finding And Order Second QME Panel (Represented Case)
Finding And Order Second QME Panel (Represented Case)
California/Workers Comp/General/ -
 Supplement Job Displacement Nontransferable Training Voucher (Between 1-1-04 And 12-31-12)
Supplement Job Displacement Nontransferable Training Voucher (Between 1-1-04 And 12-31-12)
California/Workers Comp/General/ -
 Request For Dispute Resolution Before Administrative Director
Request For Dispute Resolution Before Administrative Director
California/Workers Comp/General/ -
 Notice Of Offer Of Modified Or Alternative Work (Between 1-1-04 And 12-31-12)
Notice Of Offer Of Modified Or Alternative Work (Between 1-1-04 And 12-31-12)
California/Workers Comp/General/ -
 Notice Of Offer Of Regular Modified Or Alternative Work (On Or After 1-1-13)
Notice Of Offer Of Regular Modified Or Alternative Work (On Or After 1-1-13)
California/Workers Comp/General/ -
 Application For Independent Medical Review
Application For Independent Medical Review
California/Workers Comp/General/ -
 Description Of Employees Job Duties
Description Of Employees Job Duties
California/Workers Comp/General/ -
 Providers Request For Second Bill Review
Providers Request For Second Bill Review
California/Workers Comp/General/ -
 Physicians Return-To-Work And Voucher Report (On Or After 1-1-13)
Physicians Return-To-Work And Voucher Report (On Or After 1-1-13)
California/Workers Comp/General/ -
 Same Day Walk Through Form (Lodi)
Same Day Walk Through Form (Lodi)
California/Workers Comp/General/ -
 Minutes Of Hearing
Minutes Of Hearing
California/Workers Comp/General/ -
 Supplement To Minutes Of Hearing
Supplement To Minutes Of Hearing
California/Workers Comp/General/ -
 Course Evaluation For Administrative Director
Course Evaluation For Administrative Director
California/Workers Comp/General/ -
 Replacement Panel Request
Replacement Panel Request
California/Workers Comp/General/ -
 Request For Factual Correction Of An Unrepresented Panel QME
Request For Factual Correction Of An Unrepresented Panel QME
California/Workers Comp/General/ -
 Notice Of Offer Of Regular Work For Injuries (Between 1-1-05 And 12-31-12)
Notice Of Offer Of Regular Work For Injuries (Between 1-1-05 And 12-31-12)
California/Workers Comp/General/ -
 Qualified Medical Evaluator Complaint Form
Qualified Medical Evaluator Complaint Form
California/Workers Comp/General/ -
 Lien Filing Fee Refund Request
Lien Filing Fee Refund Request
California/Workers Comp/General/ -
 Represented Additional Panel Proof Of Service
Represented Additional Panel Proof Of Service
California/Workers Comp/General/ -
 Unrepresented Additional Panel Proof Of Service
Unrepresented Additional Panel Proof Of Service
California/Workers Comp/General/ -
 Unrepresented Replacement Panel Proof Of Service
Unrepresented Replacement Panel Proof Of Service
California/Workers Comp/General/ -
 Minutes Of Hearing (Addendum)
Minutes Of Hearing (Addendum)
California/Workers Comp/General/ -
 Lien Conference Deposition Form
Lien Conference Deposition Form
California/Workers Comp/General/ -
 Pre-Trial Conference Statement
Pre-Trial Conference Statement
California/Workers Comp/General/ -
 Pre-Trial Conference Statement Lien Issues Addendum
Pre-Trial Conference Statement Lien Issues Addendum
California/Workers Comp/General/ -
 Request For Authorization For Medical Treatment
Request For Authorization For Medical Treatment
California/Workers Comp/General/ -
 Request For Independent Bill Review
Request For Independent Bill Review
California/Workers Comp/General/ -
 Doctors First Report Of Occupational Injury Or Illness
Doctors First Report Of Occupational Injury Or Illness
California/Workers Comp/General/ -
 Finding And Order Re Replacement QME Panel Pursuant To 8 CCR 31.5 (Represented Case)
Finding And Order Re Replacement QME Panel Pursuant To 8 CCR 31.5 (Represented Case)
California/Workers Comp/General/ -
 DWC Medical Provider Network Complaint Form
DWC Medical Provider Network Complaint Form
California/Workers Comp/General/ -
 DWC Petition For Suspension Or Revocation Of Medical Provider Network (Part A)
DWC Petition For Suspension Or Revocation Of Medical Provider Network (Part A)
California/Workers Comp/General/ -
 DWC Petition For Suspension Or Revocation Of Medical Provider Network (Part B)
DWC Petition For Suspension Or Revocation Of Medical Provider Network (Part B)
California/Workers Comp/General/ -
 Notice Of Medical Provider Network Plan Modification 9767.8
Notice Of Medical Provider Network Plan Modification 9767.8
California/Workers Comp/General/ -
 Application (Petition) For Benefits For Serious And Willful Misconduct Of Employer
Application (Petition) For Benefits For Serious And Willful Misconduct Of Employer
California/Workers Comp/General/ -
 Application (Petition) For Discrimination Benefits Pursuant To Labor Code Section 132a
Application (Petition) For Discrimination Benefits Pursuant To Labor Code Section 132a
California/Workers Comp/General/ -
 Verification (Application For Discrimination Benefits Pursuant To Labor Code Section 132a)
Verification (Application For Discrimination Benefits Pursuant To Labor Code Section 132a)
California/Workers Comp/General/ -
 Verification (Commutation Of Future Payments)
Verification (Commutation Of Future Payments)
California/Workers Comp/General/ -
 Verification (Petition For Benefits For Serious And Willful Misconduct Of Employer)
Verification (Petition For Benefits For Serious And Willful Misconduct Of Employer)
California/Workers Comp/General/ -
 Verification (Petition To Reopen)
Verification (Petition To Reopen)
California/Workers Comp/General/ -
 Verification Form
Verification Form
California/Workers Comp/General/ -
 Petition Appealing Administrative Directors Independent Medical Review Determination
Petition Appealing Administrative Directors Independent Medical Review Determination
California/Workers Comp/General/ -
 Walk Through Appearance Sheet (Santa Ana)
Walk Through Appearance Sheet (Santa Ana)
California/Workers Comp/General/ -
 Workers Compensation Claim Form (DWC 1) And Notice Of Potential Eligibility
Workers Compensation Claim Form (DWC 1) And Notice Of Potential Eligibility
California/Workers Comp/General/ -
 Physicians Guide Order Form
Physicians Guide Order Form
California/Workers Comp/General/ -
 Walk Through Appearance Sheet (San Diego District)
Walk Through Appearance Sheet (San Diego District)
California/Workers Comp/General/ -
 Walk Through Hearing Request (Lodi)
Walk Through Hearing Request (Lodi)
California/Workers Comp/General/ -
 Minutes Of Hearing-Order-Order And Decision On Request For Continuance (San Diego)
Minutes Of Hearing-Order-Order And Decision On Request For Continuance (San Diego)
California/6 Workers Comp/General/ -
 Stipulation And Award And Or Order
Stipulation And Award And Or Order
California/6 Workers Comp/General/ -
 10874 Verification To Filing Of Declaration Of Readiness By Or On Behalf Of Lien Claimant
10874 Verification To Filing Of Declaration Of Readiness By Or On Behalf Of Lien Claimant
California/Workers Comp/General/ -
 Order Approving Compromise And Release
Order Approving Compromise And Release
California/6 Workers Comp/General/ -
 Minutes Of Hearing (Lodi)
Minutes Of Hearing (Lodi)
California/6 Workers Comp/General/ -
 Award (Lodi)
Award (Lodi)
California/6 Workers Comp/General/ -
 Stipulation And Award And Or Order (Lodi)
Stipulation And Award And Or Order (Lodi)
California/6 Workers Comp/General/ -
 Stipulation And Order (Replacement PQME List) (Lodi)
Stipulation And Order (Replacement PQME List) (Lodi)
California/6 Workers Comp/General/ -
 Joint Order Approving Compromise And Release Lodi)
Joint Order Approving Compromise And Release Lodi)
California/6 Workers Comp/General/ -
 Affidavit Of Defendant Re Resolution Of Liens
Affidavit Of Defendant Re Resolution Of Liens
California/6 Workers Comp/General/ -
 Disclosure Of Contract Reimbursement Rate
Disclosure Of Contract Reimbursement Rate
California/6 Workers Comp/General/ -
 Notice Of Intention To Dismiss Lien For Failure To Appear
Notice Of Intention To Dismiss Lien For Failure To Appear
California/Workers Comp/General/ -
 Utilization Review (UR) Complaint Form
Utilization Review (UR) Complaint Form
California/Workers Comp/General/ -
 Licensing Information (Home Care Organization Licensee Applicant Information)
Licensing Information (Home Care Organization Licensee Applicant Information)
California/6 Workers Comp/General/ -
 Medical Mileage Expense Form (For Travel On Or After 7-1-22)
Medical Mileage Expense Form (For Travel On Or After 7-1-22)
California/Workers Comp/General/ -
 Request For Public Records
Request For Public Records
California/Workers Comp/General/ -
 Audit Complaint Form
Audit Complaint Form
California/Workers Comp/General/ -
 Additional Panel Request
Additional Panel Request
California/Workers Comp/General/ -
 Registration For QME Competency Examination
Registration For QME Competency Examination
California/Workers Comp/General/ -
 Annual Report Of Adjusting Locations
Annual Report Of Adjusting Locations
California/Workers Comp/General/ -
 Notice To Employees-Injuries Caused By Work
Notice To Employees-Injuries Caused By Work
California/Workers Comp/General/ -
 Supplemental Job Displacement Non-Transferable Voucher (On Or After 1-1-13)
Supplemental Job Displacement Non-Transferable Voucher (On Or After 1-1-13)
California/Workers Comp/General/ -
 Medical Mileage Expense Form (For Travel On Or After 1-1-25)
Medical Mileage Expense Form (For Travel On Or After 1-1-25)
California/Workers Comp/General/ -
 Subpoena For Personal Appearance At Video Hearing (Attorney)
Subpoena For Personal Appearance At Video Hearing (Attorney)
California/6 Workers Comp/General/ -
 Subpoena Re Deposition
Subpoena Re Deposition
California/6 Workers Comp/General/ -
 OSHAB Appeal Form
OSHAB Appeal Form
California/Workers Comp/General/ -
 Subpoena Duces Tecum (Attorney)
Subpoena Duces Tecum (Attorney)
California/6 Workers Comp/General/ -
 Arbitrator Application
Arbitrator Application
California/Workers Comp/General/
Form Preview
Contact Us
Success: Your message was sent.
Thank you!







