Last updated: 7/8/2020
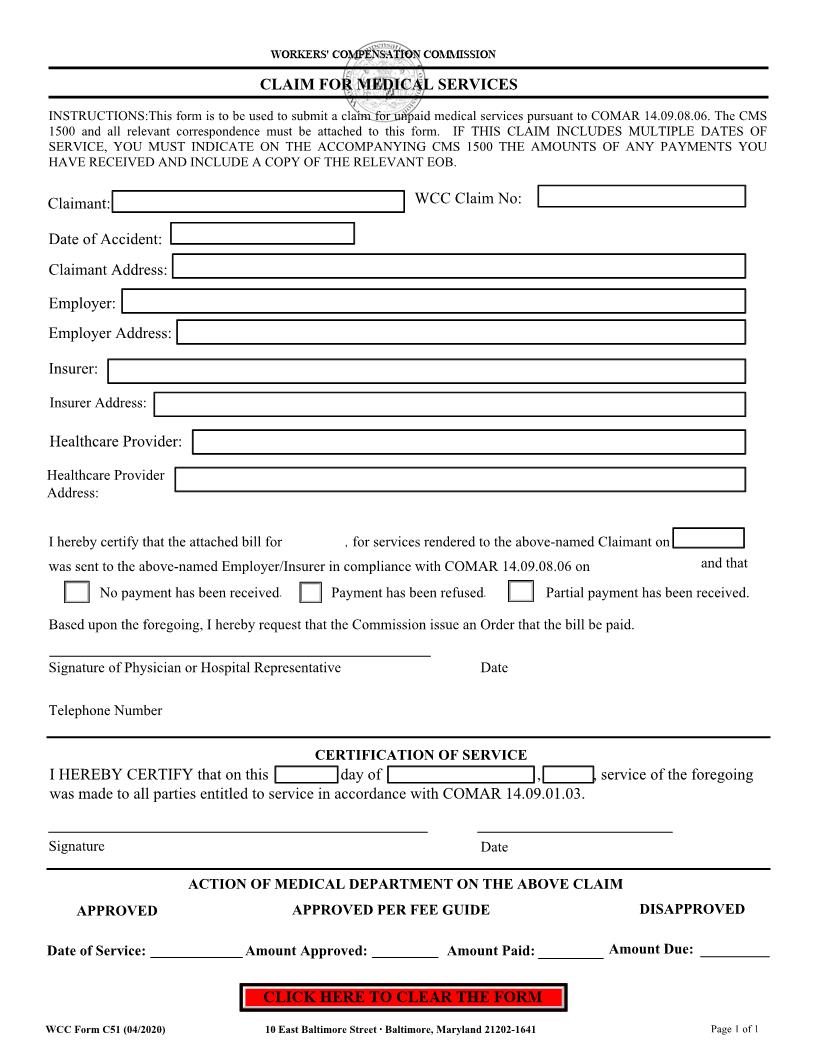
Claim For Medical Services {C-51}
Start Your Free Trial $ 13.99What you get:
- Instant access to fillable Microsoft Word or PDF forms.
- Minimize the risk of using outdated forms and eliminate rejected fillings.
- Largest forms database in the USA with more than 80,000 federal, state and agency forms.
- Download, edit, auto-fill multiple forms at once in MS Word using our Forms Workflow Ribbon
- Trusted by 1,000s of Attorneys and Legal Professionals
Description
WORKERS' COMPENSATION COMMISSION CLAIM FOR MEDICAL SERVICES INSTRUCTIONS:This form is to be used to submit a claim for unpaid medical services pursuant to COMAR 14.09.08.06. All relevant correspondence must be attached. IF THIS CLAIM INCLUDES MULTIPLE DATES OF SERVICE, YOU MUST INDICATE ON THE ACCOMPANYING CMS 1500 THE AMOUNTS OF ANY PAYMENTS YOU HAVE RECEIVED AND INCLUDE A COPY OF THE RELEVANT EOB. WCC Claim No: Claimant: Street Employer: Street Insurer: Street Healthcare Provider: Date of Accident: Social Security Number: City State ZIP City State ZIP City State ZIP Street I hereby certify that the attached bill for $ City State ZIP , for services rendered to the above-named Claimant on and that was mailed to the above-named Employer/Insurer in compliance with COMAR 14.09.08.06 on No payment has been received. Payment has been refused. Partial payment has been received. Based upon the foregoing, I hereby request that the Commission issue an Order that the bill be paid. (Signature of Physician or Hospital Representative) (Telephone Number) CERTIFICATION OF SERVICE , , I mailed, postage prepaid, a copy of the foregoing Claim I hereby certify that on the day of For Medical Services and any attached documentation to all parties and their attorneys. Signature Date ACTION OF MEDICAL DEPARTMENT ON THE ABOVE CLAIM APPROVED Date of Service: APPROVED PER FEE GUIDE Amount Approved: Amount Paid: DISAPPROVED Amount Due: Date 10 East Baltimore Street Baltimore, Maryland 21202-1641 410-864-5100 Email: info@wcc.state.md.us Web: http://www.wcc.state.md.us WCC Form C51 (03/2014) American LegalNet, Inc. www.FormsWorkFlow.com COMAR 14.09.08.06 .06 Reimbursement Procedures. A. To obtain reimbursement under this chapter, an authorized provider shall: (1) Complete Form CMS-1500 in accordance with the written instructions posted on the Commission's website; and (2) Submit to the employer or insurer the completed Form CMS-1500, which shall include: (a) An itemized list of each service; (b) The diagnosis relative to each service; (c) The medical records related to the service being billed; (d) The appropriate CPT/HCPCS code with CPT modifiers, if any, for each service; (e) The date of each service; (f) The specific fee charged for each service; (g) The tax ID number of the provider; (h) The professional license number of the provider; and (i) The National Provider Identifier (NPI) of the provider. B. Modifiers. (1) Modifying circumstances may be identified by use of the relevant CPT modifier in effect when the medical service or treatment was provided. (2) The identification of modifying circumstances does not imply or guarantee that a provider will receive reimbursement as billed. C. Time for Reimbursement. Reimbursement by the employer or insurer shall be made within 45 days of the date on which the Form CMS-1500 was received by the employer or insurer, unless the claim for treatment or services is denied in full or in part under §G of this regulation. D. Untimely Reimbursement. If an employer or insurer does not pay the fee calculated under this chapter or file a notice of denial of reimbursement, within 45 days of receipt of the CMS-1500, the Commission may assess a fine against the employer or its insurer, and award interest to the provider in accordance with Labor and Employment Article, §§9-663 and 9-664, Annotated Code of Maryland, and COMAR 14.09.06.02 E. Denial of Reimbursement. (1) If an employer or insurer denies, in full or in part, a claim for treatment or services, the employer or insurer shall: (a) Notify the provider of the reasons for the denial in writing; and (b) Mail the notice of denial of reimbursement to the provider within 45 days of the date on which Form CMS-1500 was received. (2) An employer or insurer who fails to file a notice of denial of reimbursement within 45 days of receipt of the CMS-1500 waives the right to deny reimbursement, and is subject to the provisions of Labor and Employment Article, §§9-663 and 9664, Annotated Code of Maryland, and COMAR 14.09.06.02 F. Objection to Denial of Reimbursement. (1) A provider may contest a partial or total denial of reimbursement, by submitting to the Commission the following items: (a) A "Claim for Medical Services" on a form provided by the Commission; (b) The Form CMS-1500 that relates to the unpaid claims; and (c) All correspondence relating to the unpaid claim. (2) The Commission shall review the items submitted, without hearing, and issue its decision in an Order Nisi. G. Hearing on Objection to Commission's Order Nisi. (1) The provider, employer, or insurer may contest the Commission's Order Nisi by filing with the Commission a controversion of medical claim, on a form provided by the Commission, within 30 days of the date of the Order Nisi. (2) The Commission shall schedule a hearing on the matter and render a decision. American LegalNet, Inc. www.FormsWorkFlow.com








