Last updated: 1/28/2020
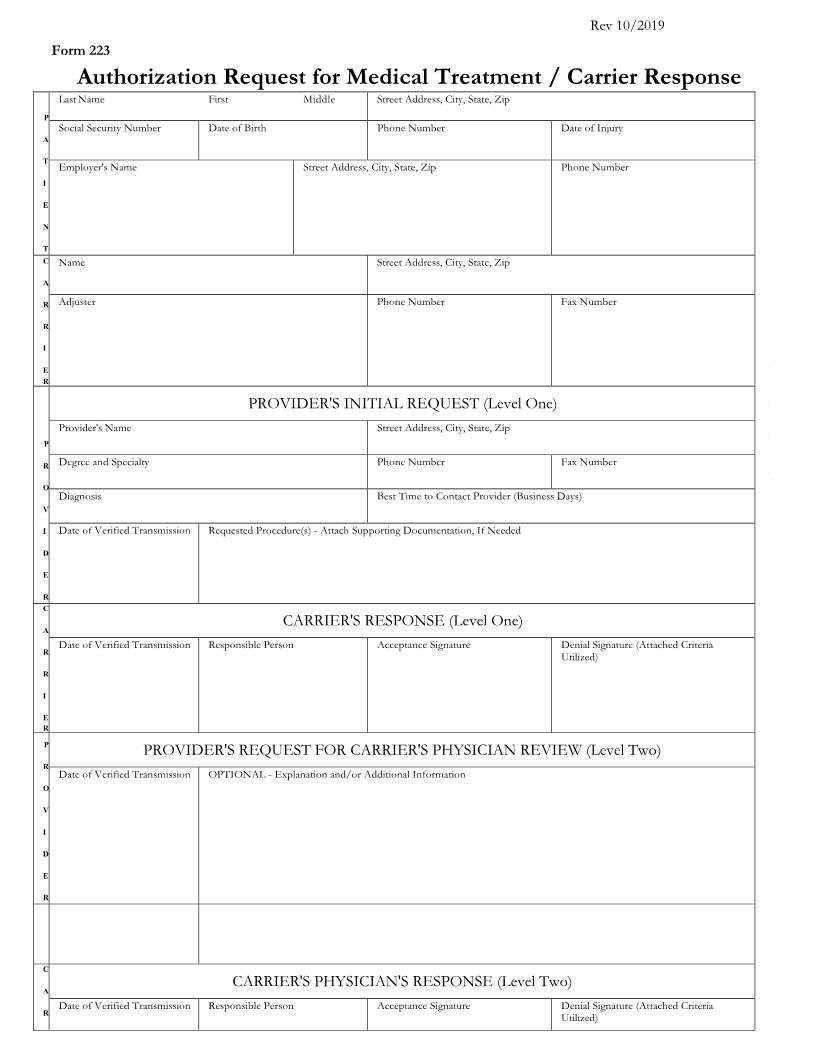
Authorization Request For Medical Treatment Carrier Response {223}
Start Your Free Trial $ 13.99What you get:
- Instant access to fillable Microsoft Word or PDF forms.
- Minimize the risk of using outdated forms and eliminate rejected fillings.
- Largest forms database in the USA with more than 80,000 federal, state and agency forms.
- Download, edit, auto-fill multiple forms at once in MS Word using our Forms Workflow Ribbon
- Trusted by 1,000s of Attorneys and Legal Professionals
Description
Form 223 Authorization Request for Medical Procedures / Carrier Response PLEASE PRINT OR TYPE First Middle Street Address, City, State, Zip Last Name P A T I E N T Social Security Number Date of Birth Phone Number Date of Injury Employer's Name Street Address, City, State, Zip Phone Number C A R R I E R Name Street Address, City, State, Zip Adjustor Phone Number Fax Number PROVIDER'S INITIAL REQUEST (Level One) Provider's name Street Address, City, State, Zip P R O V I D E R Degree and Specialty Phone Number Fax Number Diagnosis Best Time to Contact Provider (Business Days) Date of Verified Transmission Requested Procedure(s) Supportive Documentation Attached If Needed C A R R I E R P R O V I D E R C A R R I E R CARRIER'S RESPONSE (Level One) Date of Verified Transmission Responsible Person Acceptance Signature Denial Signature(Attach Criteria Utilized) PROVIDER'S REQUEST FOR CARRIER'S PHYSICIAN REVIEW (Level Two) Date of Verified Transmission OPTIONAL - Explanation and/or Additional Information CARRIER'S PHYSICIAN'S RESPONSE (Level Two) Date of Verified Transmission Name of Responsible Physician Acceptance Signature Denial Signature(Attach Criteria Utilized) If denied, a copy of this form must be faxed to the Labor Commission P A T I E N T PATIENT'S ACKNOWLEDGMENT OF RESPONSIBILITY IF PROCEDURE IS DENIED BY CARRIER I agree that I may become liable for the cost of the medical procedure if it is ultimately determined to not be compensable Date Patient's Signature NOTICE TO CLAIMANT: If you are in disagreement with the carrier and cannot resolve your differences by talking with the carrier and/or your treating physician, you should then call the Labor Commission, Division of Industrial Accidents, for further instructions. Official Form 223 Revised 10/14 State of Utah * Labor Commission * Division of Industrial Accidents 160 East 300 South * P O Box 146610 Salt Lake City, UT 84114-6610 * Telephone: 801-530-6800 American LegalNet, Inc. Fax: 80-530-6804 * Toll Free: (800) 530-5090 * www.laborcommission.utah.gov www.FormsWorkFlow.com The use of Form 223 is governed by the Division of Industrial Accident's Rule R612-300-11, Utilization Review Standards." A treating physician may use Form 223 to request authorization for payment for a course of proposed treatment, including surgery, hospitalization or any diagnostic study beyond plain X-rays. Levels of Review Level I The treating physician sends this form with the Provider Request portion completed, along with documentation for the requested procedure, to the payer of the claim. The payer is to notify the treating physician within five (5) business days of approval or denial of the request. The payer may use medical or non medical personnel at this level to make the decision to approve or deny the request. If the request is denied the payer must send the criteria used in making the decision to deny payment for the procedure requested. Level II A physician who has been denied authorization for payment for treatment, or has received no response to the request within the five (5) days, may request physician review of the request by sending the completed portion of the request for physician review. The requesting physician is to include the days and times that he/she is available to discuss the case with a reviewing physician. The payer's physician reviewer must make a reasonable attempt to contact the treating physician regarding the payer's denial and must complete the review within five (5) business days of the treating physician's request for review. If the authorization for payment for the treatment is denied, the reviewing physician must send the criteria used to make the decision along with the name and specialty of the reviewing physician to the treating physician. If the treating physician proceeds with the treatment without the approval of the payer and the treatment is a non emergency, the payer is liable for only 75% of the amount otherwise payable if the Labor Commission deems the treatment reasonable to treat the industrial injury. The 25% reduction does not apply if the treating physician receives authorization from the injured worker's health insurance plan. For a complete text of the rule you may access the rule (R612-300-11) through the Labor Commission's Web site at www.laborcommission.utah.gov. American LegalNet, Inc. www.FormsWorkFlow.com








